
Osteochondrosis of the cervical spine or cervical osteochondrosis is a disease of degenerative-dystrophic origin that affects the intervertebral discs and cervical vertebrae with the formation of protrusions and intervertebral hernias, which eventually leads to dysfunction of the spinal cord and is often the cause of the patient's disability.
Features of the structure of the cervical spine
The vertebrae are the bones that make up the spine. Each vertebra has a body that carries the entire load, the vertebral arch, transverse and spinous processes.

The vertebral arches of the vertebrae form the vertebral canal in which the spinal cord runs. The processes of the spine are designed to anchor the back muscles.
There are also anterior and posterior ligaments that connect the vertebrae together.
The intervertebral disc is a rounded flat structure made up of an annulus fibrosus and a nucleus pulposus, the main function of which is to absorb shock. The intervertebral discs lie between the vertebrae.
The facet joint is a flexible connection between the processes of two adjacent vertebrae. The facet joints give the spine flexibility.
Intervertebral foramen are foramina that are formed by structural elements (legs, articular processes) of two adjacent vertebrae and are intended for the exit of the radicular nerves of the spinal cord.
There are paravertebral muscles that support the spine and its various movements.
The cervical spine is the uppermost and most flexible part of the spine, which consists of seven vertebrae and has a C-shape due to its pre-bend (cervical lordosis).
All head movements - tilting, turning, circling - are performed from this part of the spine.
Interesting!In addition, the cervical spine is the most traumatized part, as the cervical vertebrae have low strength and weak muscular apparatus compared to others.
Osteochondrosis of the cervical spine is common for the same reason.
Prevalence of cervical osteochondrosis
Osteochondrosis of the cervical spine affects the working age population over 30 years of age. This disease is more common in women than men.
According to the World Health Organization, 40-90% of the world's population suffer from osteochondrosis.
Important!Every second patient with osteochondrosis has dystrophic and degenerative changes in the spine in the cervical spine.
Causes of osteochondrosis of the cervical spine
Osteochondrosis can be seen as a tribute to a person's ability to stand and walk on two legs. This opinion is confirmed by the fact that not a single animal that walks on four legs suffers from osteochondrosis.
Despite the availability of modern methods of diagnosing diseases and a deep knowledge of human anatomy and physiology, the specific causes of osteochondrosis have not yet been established.

However, reliable factors are known that lead to degenerative-dystrophic changes in the spine. These include the following:
- insufficiently mobile lifestyle of a person, which leads to a weakening of the muscular apparatus of the back. Often office workers, cashiers, salespeople and drivers suffer from osteochondrosis;
- Hard physical work;
- mechanical injury to the back;
- genetic predisposition to osteochondrosis;
- Overweight and obesity;
- neuropsychic stress;
- improper exercise in the gym;
- Beriberi, micronutrient deficiency, metabolic disorders;
- wrong diet;
- the presence of diseases of the kidneys, digestive and endocrine systems;
- Infectious diseases;
- frequent hypothermia of the body;
- congenital and acquired immunodeficiencies.
Pathogenesis (mechanism of development) of cervical osteochondrosis

Almost all factors that contribute to the development of osteochondrosis lead to spasms in the back muscles. Muscle spasms, in turn, disrupt the blood supply and metabolism of the bone tissue of the vertebrae and intervertebral discs.
This leads to dystrophic changes, i. e. dehydration, dehydration and loss of elasticity of the vertebrae and intervertebral discs.
A further load on the spine leads to a flattening, protrusion (protrusion over the annulus fibrosus) of the intervertebral discs.
No less important in the pathogenesis of cervical osteochondrosis is the burden of holding and moving the head.
The strain on the cervical vertebrae is enormous, as the average head weight is 3-5 kg and, unfortunately, their bone tissue is fragile and thin.
The development of osteochondrosis is also made easier by technological advances - smartphones, tablets, e-books, if you bend down while using these devices.
The intervertebral discs cannot efficiently amortize the spine, so compensation mechanisms are triggered.
Important!One of these mechanisms is osteophyte multiplication and the development of spondylosis.
False joints can also form along the back surface of the vertebrae of the cervical spine - uncovertebral osteoarthritis.
All of these processes eventually lead to a decrease in cervical lordosis (hypordosis), bulges, and intervertebral discs, which sooner or later become the main cause of a person's disability or require urgent surgical treatment.
The pathogenesis of cervical osteochondrosis can be divided into four stages:
- Onset of instability of the cervical vertebrae;
- The formation of protrusions of the intervertebral discs, a decrease in the intervertebral spaces, the beginning of the destruction of the annulus fibrosus, which leads to pinching of the nerves, which is manifested in neck pain;
- The annulus fibrosus is completely destroyed and the nucleus pulposus protrudes beyond its limits, so that a herniated disc forms and the spine is deformed;
- Stage of disability. The eddies grow together. Patients find it difficult to move. Sometimes the condition can improve, but not for long.
Symptoms and syndromes of osteochondrosis of the cervical spine

The main symptoms of cervical osteochondrosis include:
- persistent neck pain of a throbbing or aching nature that can spread to the back of the head, eye sockets, ears, and shoulder girdle;
- Upper limb pain that increases with movement;
- stiff movements of the upper limbs, violation of their sensitivity (tingling, burning, numbness), weakening of muscle strength;
- morning stiffness in the neck;
- Pain in the cervical spine when moving the head;
- periodic dizziness with cervical osteochondrosis, darkening of the eyes, unconsciousness with sharp turns of the head;
- Feeling of tinnitus;
- Hearing and visual impairment;
- Numbness and tingling of the tongue;
- Cardialgia (heart pain), sometimes confusing cervical osteochondrosis with acute coronary syndrome. The difference lies in the lack of effectiveness of nitrates;
- Due to microcirculation disorders and tissue oxygen deficiency, connective tissue in the cervical spine, the so-called "withers", increases.
All symptoms of cervical osteochondrosis can be grouped into the following syndromes:

- Reflex;
- radicular;
- radicular-vascular;
- Spinal compression;
- cerebral.
Reflex syndrome consists of cervicalgia - severe pain in the neck, due to which the patient is forced to fix the head and strain the muscles of the neck.
Feeling the spinous processes, paravertebral points and intervertebral discs brings and / or increases pain.
Reflex syndrome is also characterized by pain in the upper limbs, in the back of the head, or in the temporal regions of the head.
Radicular syndrome is a combination of sharp acute pain that increases with head movements and is caused by pinching nerves in the intervertebral foramen.
The radicular-vascular syndrome is characterized by vegetative-trophic disorders in the form of humerus-scapular periarthritis.
The patient worries about pain in the shoulder joint, stiffness of movement, impaired skin sensitivity, swelling of the hand and wrist. In addition, the patient cannot bring his hands back.
Spinal compression syndrome occurs due to compression of the spinal cord and its vascular system. Herniated discs, osteophytes, thickening of the yellow ligament can lead to this.
Interesting!The patients have pain in the neck and shoulder area, flaccid paresis of the upper extremities and spastic paresis of the lower extremities, sensory disorders.
The cerebral syndrome with cervical osteochondrosis combines several such syndromes:
- diencephalic syndrome - increased irritability, neurasthenia, general weakness, insomnia, absent-mindedness. In severe cases, anxiety, numbness of the upper and lower extremities, increased sweating, chills appear;
- posterior cervical sympathetic Barre syndrome or "cervical migraine" - severe headache, as in migraine in one half of the head against the background of dizziness, visual and hearing impairments, numbness in the hands.
- Syncope syndrome - fainting with a sharp turn of the head;
- vestibular stem and cochlear stem syndromes - dizziness, unsteadiness when walking, nausea, and even vomiting;
- Visual disturbance syndrome - deterioration in vision, visual disturbance, flashes of "dots", "flies" in front of the eyes.
Diagnosis of osteochondrosis of the cervical spine

Like any diagnosis in medicine, the diagnosis of osteochondrosis of the cervical spine is made on the basis of the patient's complaints, medical history, examination and research auxiliary methods.
In addition to the clinical examination, the patient must undergo the following methods:
- X-ray of the cervical spine;
- Computed tomography of the cervical spine;
- Magnetic resonance imaging of the cervical spine;
- Doppler ultrasound examination of the neck vessels;
After the diagnostic measures, the doctor chooses the treatment tactics based on the results of the diagnosis and analysis.
Treatment of osteochondrosis of the cervical spine
Treatment of osteochondrosis of the cervical spine consists in the elimination of the radicular syndrome and the elimination of the inflammatory process.

In the acute phase of the disease, you need to adhere to strict bed rest. The soft mattress should be replaced by a hard one or a wooden sign should be placed over it.
Drug therapy for cervical osteochondrosis is carried out with the following groups of drugs:
- Non-steroidal anti-inflammatory drugs;
- Drugs of the chondroprotective group;
- Pain relievers and anti-inflammatory gels and ointments;
- Vitamin preparations - ascorbic acid, retinol acetate, tocopherol acetate;
- Calcium supplements;
- Drugs that improve tissue microcirculation;
- Muscle relaxants.
Treatment for cervical osteochondrosis includes the following methods:
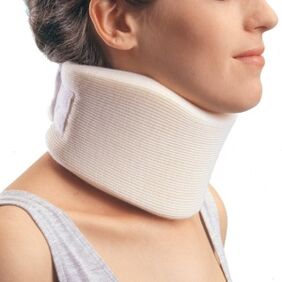
- Wearing a special collar around the neck, which not only relieves the neck, but also restricts movement;
- Stretching with a Glisson loop - the head of the patient lying on the bed is fixed with a Glisson loop and the head of the bed is raised by 20-30 cm. This process relaxes the muscle corset of the spine, increases the intervertebral fissures, releases pinched nerves;
- Manual therapy for cervical osteochondrosis should only be performed by an experienced manual therapist. Manual therapy is performed using relaxing and segmental massage techniques, mobilization that restores damaged joint functions, and manipulations to restore the joints to full range of motion.
- physiotherapeutic methods in osteochondrosis of the cervical spine - diadynamic therapy, electrotherapy, laser therapy, shock wave therapy, balneotherapy, treatment with ultrasound and ultraviolet rays, magnetic therapy and other methods.
- Physiotherapy for cervical osteochondrosis includes exercises to strengthen the muscle corset. Exercise is useful not only for treating osteochondrosis, but also for prevention. They can be done before bed at home, at the gym, at work, and at school during breaks.
Surgical treatment of cervical osteochondrosis
Treatment with surgical methods is indicated in severe radicular syndrome that cannot be relieved by medication, with an increase in motor and sensory functions of the upper limbs, as well as with compression of the spinal cord.
Important!Operations to remove herniated discs and osteophytes are common.
Prevention of osteochondrosis of the cervical spine

- healthy sleep on an orthopedic mattress;
- use a low pillow;
- regularly visit the sauna or bath. Steam perfectly relaxes the neck muscles;
- You need to take a hot shower for at least 10 minutes each day.
- Do sports, do gymnastics, go for a walk. Swimming, yoga, and Pilates are ideal for this;
- all head movements should be precise, with no sharp turns;
- Correctly distribute the load on the spine during physical work and sports;
- Take breaks and warm up while sitting down;
- maintain proper posture when sitting at a table or computer;
- Chairs and a table should match your height.





















